Introduction
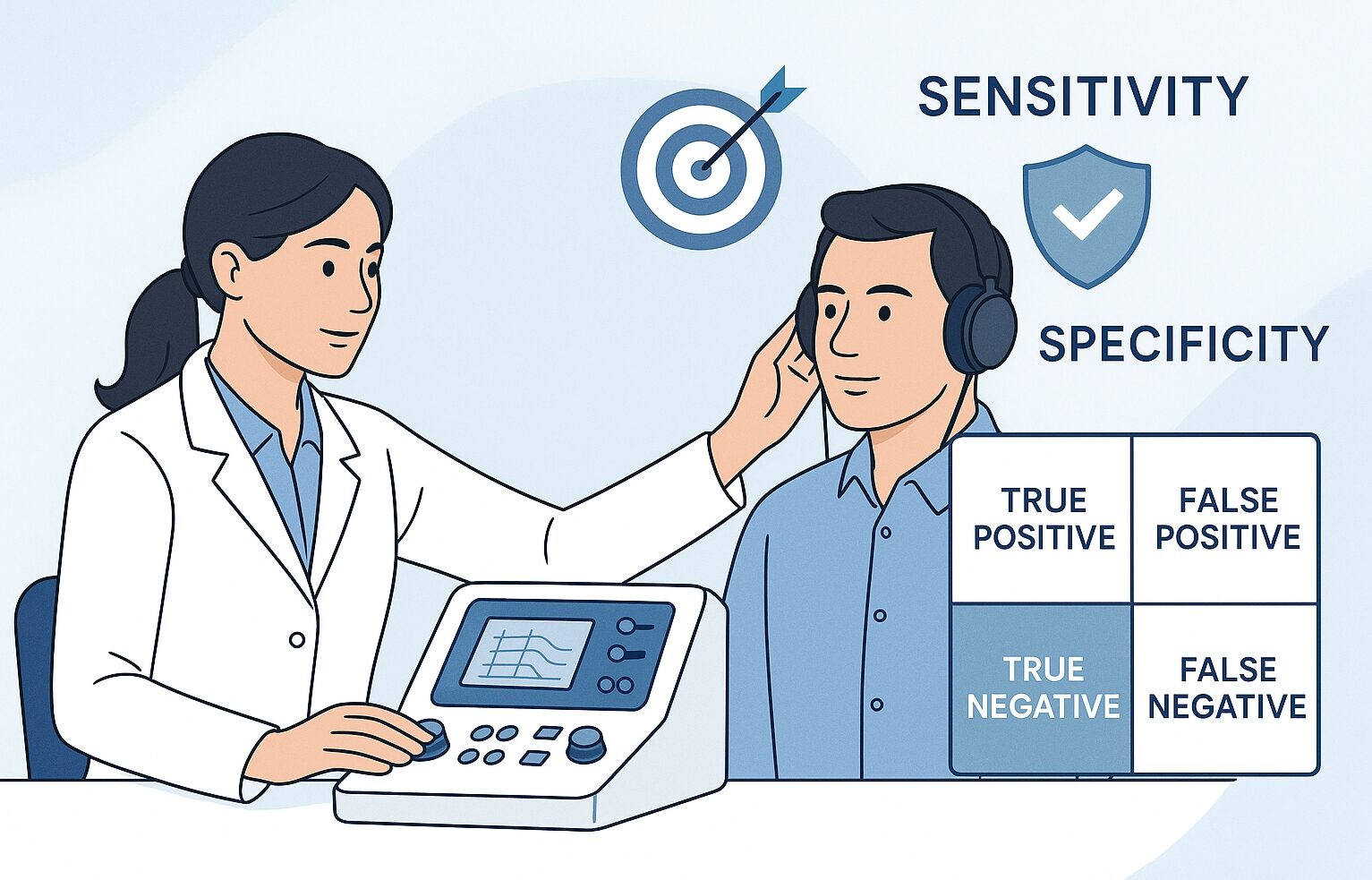
As an audiologist, you’ve likely encountered terms like “sensitivity,” “specificity,” and “false positive” in research papers and clinical guidelines. But what do these terms really mean for your practice and your patients? These concepts help us understand how accurate a screening or diagnostic test really is.
Let’s break them down in simple terms—with examples from audiological practice.
Why Test Accuracy Matters in Audiology
Before diving into the technical terms, let’s consider why understanding test accuracy is crucial in our field:
- Patient Trust: When we explain test results clearly, patients develop greater confidence in our diagnoses and recommendations.
- Resource Allocation: Accurate testing helps ensure that limited healthcare resources are directed to those who truly need intervention.
- Clinical Decision-Making: Understanding test limitations allows for better clinical judgment when interpreting results.
- Research Applications: Knowledge of these concepts helps us critically evaluate new screening and diagnostic tools.
The Four Outcomes of Any Audiological Test

Every hearing test essentially produces one of four possible outcomes when compared to the true hearing status of a patient:
1. True Positive (The “Hit”)
A true positive occurs when our test correctly identifies a hearing loss that actually exists. This is what we aim for as clinicians—a clear “hit” that allows us to provide appropriate intervention.
Real-world example: A newborn fails an automated auditory brainstem response (AABR) screening, and subsequent diagnostic testing confirms a moderate sensorineural hearing loss.
2. False Positive (The “False Alarm”)
A false positive happens when our test indicates hearing loss in someone who actually has normal hearing. This can cause unnecessary worry and follow-up testing.
Real-world example: Environmental noise during a screening test causes a child to fail the screening, but comprehensive diagnostic testing reveals normal hearing.
3. False Negative (The “Miss”)
Perhaps the most concerning outcome is the false negative, where our test suggests normal hearing in someone who actually has hearing loss. This “miss” can delay crucial intervention.
Real-world example: A screening test fails to detect a mild high-frequency hearing loss in a school-aged child, potentially affecting their classroom performance.
4. True Negative (The “Correct Rejection”)
A true negative occurs when our test correctly identifies normal hearing in someone who does indeed have normal hearing. Along with true positives, this is our desired outcome.
Real-world example: An adult passes a pure-tone screening test and truly has normal hearing sensitivity.
Sensitivity: Catching the Real Hearing Losses
Sensitivity measures how well a test identifies those who truly have hearing loss. It’s the percentage of individuals with hearing loss who are correctly identified by the test.
In other words:
If 100 people actually have hearing loss, and your test detects 90 of them, the sensitivity is 90%.
High sensitivity = few misses (false negatives).
Formula: Sensitivity = True Positives ÷ (True Positives + False Negatives)
In simple terms: How good is the test at catching actual hearing loss?
A test with high sensitivity rarely misses cases of hearing loss. For newborn hearing screening programs, high sensitivity is crucial because we don’t want to miss any babies with hearing loss, as early intervention is vital for language development.
Specificity: Avoiding False Alarms
Specificity measures how accurately a test identifies those without hearing loss. It’s the percentage of individuals with normal hearing who are correctly identified as having normal hearing.
In other words :
If 100 people do not have hearing loss, and your test correctly identifies 95 of them, the specificity is 95%.
High specificity = few false alarms (false positives).
Formula: Specificity = True Negatives ÷ (True Negatives + False Positives)
In simple terms: How good is the test at avoiding false alarms?
A test with high specificity rarely misdiagnose someone with normal hearing as having hearing loss. This helps reduce anxiety, unnecessary follow-up testing, and wasted resources.
The Trade-off Between Sensitivity and Specificity
Here’s where things get interesting—and sometimes challenging—in clinical practice. There’s often a trade-off between sensitivity and specificity:
- Lower screening thresholds (e.g., testing at 15 dB HL instead of 25 dB HL) increase sensitivity (catch more hearing losses) but decrease specificity (more false alarms).
- Higher screening thresholds (e.g., testing at 30 dB HL instead of 25 dB HL) increase specificity (fewer false alarms) but decrease sensitivity (more missed hearing losses).
As audiologists, we must decide which is more important for each specific clinical scenario.
Practical Tips for Improving Test Accuracy
- Minimize environmental noise: Ensure your testing environment meets appropriate standards to reduce false positive results.
- Maintain and calibrate equipment regularly: Even small deviations in equipment performance can affect test accuracy.
- Consider multiple test methods: Different tests have different strengths—OAEs may better detect cochlear dysfunction, while pure-tone audiometry directly measures behavioral response to sound.
- Train personnel thoroughly: Proper test administration is crucial for accuracy, especially for screening conducted by non-audiologists.
- Document test conditions: Note any factors that might influence results, such as patient cooperation or unusual background noise.
Conclusion: Beyond the Numbers
While understanding sensitivity, specificity, and related statistical measures is important, remember that behind every data point is a real person. The true value of audiological testing lies not just in its statistical accuracy but in how effectively it helps us connect patients with appropriate care.
These concepts, will help you make more informed clinical decisions, and most importantly, communicate more effectively with your patients about what their test results really mean for their hearing health.
[…] A hearing screening is essentially a quick “pass” or “fail” assessment designed to identify individuals who may have hearing loss and require further evaluation. I have discussed screening outcomes in details in the last post […]
[…] two often go hand-in-hand and are crucial for diagnostic accuracy. In one of the previous we have discussed these terms and other related terms in […]